This work was done by LaGuardia student Sara El Houzaly under the supervision of Dr. Richa Gupta, from the Natural Sciences department.
This research was supported by the NIH Bridges program. Dr. Richa Gupta served as the Principal Investigator and Research Mentor, and Sara El Houzaly was supported by the NIH Bridges Undergraduate Research Scholarship through it.
The effects of climate change are evident worldwide as average global land and air temperatures have been rising, glaciers and ice sheets are shrinking with the concomitant rise in sea levels, extreme weather events have become more frequent, and oceans are warming and acidifying. Humanity is facing a big environmental challenge which not only impacts our habitat but will also have ramifications on our health. The present review describes a detailed examination of the scientific evidence proving the relationship between climate change and various fatal human diseases in different geographical regions. Our findings indicate that variations in the patterns of climatic factors, such as temperature, rainfall, and humidity, can increase the incidence of respiratory infections like tuberculosis and significantly change the incidence of waterborne diseases, such as cholera. It has also been noted that increase in the spread and longevity of mosquitos, which serve as carriers for various pathogens, can lead to high transmission rates of several vector-borne diseases. Climate change could also alter the dispersion of primary and secondary air pollutants, like nitrogen dioxide and ozone. High concentrations of these atmospheric gases closely link to the increasing rates of congestive heart failure and myocardial infarction. Furthermore, the frequency of occurrence of allergies and asthma is also likely to increase globally with climate change. Based on our studies, we recommend that characterizing emerging disease risks is crucial to evaluate our vulnerability and determine areas where public health efforts will be required with a greater focus in the coming years.
Keywords: Climate change, global warming, human diseases, infectious diseases, and environmental changes
Climate change refers to long-term alterations in weather conditions and patterns of extreme weather events. The incoming solar radiation of the sun powers our climate system, and variability in the outgoing thermal (infrared) radiation reflected by earth changes our climate. The planet's average surface temperature has risen 1.18°C since the late 19th century leading to global warming [1,2]. This change is driven mainly by the increasing carbon dioxide and methane emissions into the atmosphere due to the different human activities and burning of fossil fuels. Global warming can be explained by the greenhouse effect, which was identified by scientists as far back as 1850s and refers to the natural warming phenomenon that occurs when some gases in the earth’s lower atmosphere (comprising of two or more atoms per molecule) trap the infrared radiation i.e., heat reflected by the planet’s surface.
The main gases responsible for the greenhouse effect include carbon dioxide (CO2), methane (CH4), nitrous oxide (N20), ozone (O3), water vapor (H2O), and fluorinated gases (HCFC, SF6). The increasing atmospheric levels of greenhouse gases are leading to climate change, which has numerous negative consequences on the environment such as extreme heat waves, wildfires, rising sea-levels, changes in precipitation resulting in floods and droughts, melting of glaciers, intense hurricanes, and deteriorated air quality. Humanity is posed with a serious environmental challenge, which is affecting our health, daily lives, and our planet’s biodiversity, and therefore, demands immediate attention globally.
The focus of our paper is to discuss how, with climate change, the risk for several diseases that target different organ systems of the human body is increasing. In the sections below, we will first discuss the impact of climate change on various vector-borne and water-borne diseases. It is important to note that many of these diseases are infectious, which have the potential to spread from one host to another in local and cross border communities rapidly and in short time frames, thereby posing critical emerging concerns worldwide. Next, we will investigate how the changing climatic conditions and deteriorating air quality affect the incidence of cardiovascular diseases, such as heart attacks or cardiac failure. We will also examine how atmospheric ozone has emerged as a major health hazard in recent years and its connection to the rise in various neurological and obstructive respiratory illnesses. Finally, we will survey how other physical factors related to climate change, such as atmospheric pollen and fluctuations in temperature, humidity, or rainfall, have escalated the episodes of respiratory diseases, such as allergies and tuberculosis.
Owing to the short life cycles of several Dipteran vectors (two-winged insects or true flies), diseases spread by them can respond rapidly to weather and climate changes, contributing to severe epidemics in many cases. In general, tropical and subtropical regions have a high prevalence of diseases, such as Dengue, Malaria, Yellow fever, and Chikungunya. With global warming, an increasing spread of mosquitoes and flies has been noticed from the tropics to the higher northern/southern latitudes, and according to recent predictions, more warming will occur in the coming years and more severely toward the poles. Consequently, temperate countries are at a considerable risk of suffering outbreaks of various vector-borne diseases owing to the following reasons [3,4]: (a) due to long-term changes in temperature and rainfall patterns, endemic vector-borne diseases can become more prevalent; (b) vector-borne diseases can shift their geographic extents toward the poles, in previously unaffected temperate regions; and (c) the changing climate of the currently endemic and non-endemic regions may become more suitable for the emergence of new vector-borne diseases due to the increasing abundance of vectors and pathogens in these areas and through international migration.
Mosquitoes like Aedes aegypti and Anopheles gambiae are carriers of several pathogenic viruses and parasites which cause deadly afflictions to humans, such as Dengue, Yellow Fever, Zika and Chikungunya, and Malaria. The incidence of Malaria varies seasonally in highly endemic regions and is considered most sensitive to long-term climate change [5]. In 2020, the global load of malaria cases was ~241,000,000, with the highest proportion in Africa [6]. Malaria is a life-threatening disease transmitted by female Anopheles mosquitoes carrying Plasmodium falciparum parasites. The ideal breeding grounds for these mosquitoes are warm, humid, and rainy environments. The malaria parasites also require warm temperatures to complete their growth cycle inside the mosquitoes. Therefore, temperature, rainfall, and humidity increases can promote the growth of malaria-carrying mosquitoes at higher altitudes, increasing malaria transmission to areas where it was not prevalent previously. A study conducted in Venezuela showed that malaria rates have increased by over one-third in the year following an El Niño year, characterized by unusual winds from the Pacific Ocean causing warm equatorial surface waters to move eastward toward Central and South America [7]. Possible reasons for this high malarial transmission pattern after the previous low incidence year include a temporary reduction in the immunity level of the local population with mosquitoes preferring the high rainfall and warmer temperatures in the post-Nino year [7]. Several widely cited examples suggest that climate change has already resulted in the introduction of several infectious diseases in previously unaffected regions. In accord with this, the spread of malaria into the highland regions of East Africa was indeed reported from 1911-1995, where the high incidence of this disease was not reported earlier [8].
In the tropics, Dengue is another widespread disease with local variations in risk depending on rainfall, temperature, and unplanned rapid urbanization. Prior to 1970, only nine countries had suffered from severe Dengue epidemics; today, the disease is endemic in more than 100 countries across Africa, the Eastern Mediterranean, the Americas, the Western Pacific, and Southeast Asia. The number of cases of Dengue in the Americas, South-East Asia, and West Pacific grew from 1.2 million in 2008 to 3.2 million in 2015, and globally to 5.2 million in 2019. In addition to climate change, due to increasing populations, urbanization, and deforestation, dengue vectors are expanding their niches geographically. Previously unaffected areas are now experiencing dengue outbreaks. Globally, dengue cases remain on the rise despite numerous interventions, and dengue control faces challenges from endemic transmission in Africa and the Americas, outbreaks in Portugal, and an increase in incidences in Asia [9] In each instance, dengue transmission is increased by global warming due to the associated changes in temperature and humidity which favor proliferation of the carrier mosquitoes [10].
Increasing global temperatures cause more water to evaporate from our water bodies, resulting in higher atmospheric moisture levels, heavier and more intense rainfall, storm surges, and higher sea temperatures. These environmental changes in turn lead to flooding and runoff that spread sewage, chemicals, and disease agents. Therefore, as climate change continues, water-borne illnesses are bound to spread more, particularly in underdeveloped and developing countries [11,12]. Globally, an estimated 1.3 million to 4.0 million cases of cholera occur every year, resulting in 21,000 to 143,000 deaths [12]. Cholera is a bacterial disease, caused by Vibrio cholerae, which spread through contaminated water and are responsible for small intestinal damage. If left untreated, cholera can be fatal within hours, even in otherwise healthy people, due to severe diarrhea and dehydration. The transmission of cholera can occur through direct contact with infected people, use of contaminated water containers, unhealthy food preparation processes, or by contacting contaminated environmental reservoirs with persistent bacteria. Warmer climate also promotes the growth and proliferation of V. cholerae. In addition, rainfall directly affects the transmission of cholera, since heavy rainfall increases the possibility of treated water being contaminated with wastewater. Alternatively, low rainfall can increase the concentration of pathogens in water sources, and thus transmission directly from the environment could increase [13]. A predicted global map for the increased spread of cholera in different geographical regions via its causative bacterium, V. cholerae, in almost all seawaters by the year 2100 was recently published and presents a daunting problem [14]. Climate variables and cholera cases are positively related. According to a recent study in the Iranian province of Qom, both high temperatures and low precipitation contributed to the spread of cholera [15]. It was noted over the course of a decade, that the increase in air temperatures during the dry summers had created highly favorable environmental conditions for bacterial growth and survival. Low precipitation and increased evaporation during dry months also reduce the amount of surface and ground water. These changing climatic conditions may result in an increase in salinity, organic matter, and aqueous temperatures, ultimately increasing pathogen growth and proliferation in water resources. Thus, using contaminated and untreated water for residential consumption or watering vegetation could increase cholera incidence in vulnerable populations [11]. Further, seasonality has been found to play a significant role in the increase in cholera outbreaks during warm months. According to several studies, environmental factors are the most critical factors driving the incidence of cholera, which is corroborated by findings from East Africa, Zambia, and South China [16-18]. In these affected regions, the risk is highest for impoverished populations [11,12] living with insufficient sanitation and water supply, which can lead to mass displacements making them more susceptible to cholera outbreaks.
Climate change and air pollution are intricately linked, as many sources of air pollution also contribute to climate change. When fossil fuels are burned for energy production and transportation, harmful pollutants are released into the air along with greenhouse gases that trap heat in the atmosphere and contribute to global warming [20]. An escalating number of studies are showing a strong correlation between exposure to ambient air pollution and the increasing risk of cardiovascular diseases. A population-based study that included all long-term residents living in Ontario, Canada, aged between 35 to 85 years from 2001 to 2015 (~5.1 million), showed that long-term exposure to increasing concentrations of air pollutants, such as inhalable particulate matter of diameter ≤ 2.5 µm (PM2.5), ozone (O3) and nitrogen dioxide (NO2), are associated with increased incidence of congestive heart failure (CHF) and acute myocardial infarction (AMI) [19]. In terms of the underlying biological mechanisms, experimental studies have indicated that exposure to air pollution can lead to oxidative stress, systemic inflammation, and vasoconstriction, which may increase blood pressure (hypertension) and decrease heart rate variability and cardiac output. These effects can in turn result in vascular dysfunction, atherosclerosis and alterations in cardiac function and structure, ultimately increasing the risk of cardiovascular diseases, including AMI (commonly known as a heart attack), cardiac arrhythmia, ischemic stroke, and heart failure [20-22].
In the atmosphere, particulate matter is a mixture of solid and liquid particles that are suspended in air and vary in their sizes and chemical compositions. Particulate matter gets formed when fuel is burned, and atmospheric chemical reactions take place. Such particles have a wide range of sizes, the finer of which (PM2.5) can enter deep into the lungs and bloodstream and pose serious health risks. Population-based studies in 20 cities across the United States and 29 cities of Europe have found that the mortality rate due to cardiac affects was higher on the day following high levels of atmospheric particulate pollution. The National Morbidity, Mortality, and Air Pollution Study (NMMAPS) in the United States observed outcomes for 50 million people and reported that for every 10-μg/m3 elevation in PM10 (inhalable particulate matter of diameter ≤ 10 µm), there was an increase of 0.21% and 0.31% for daily all-cause and cardiopulmonary mortality, respectively. The study from Air Pollution and Health: A European Approach project also showed consistent results for 43 million people in Europe, indicating a spike in mortality by 0.6%, and in cardiovascular deaths by 0.69% per day, for every 10-μg/m3 increase in PM10 [23]. Various other reports have revealed connections between high levels of particulate air pollution and increased admissions to hospitals for acute coronary syndrome, including anginal chest pain and AMI. Furthermore, studies conducted on rabbits also showed that upon frequent exposure to particulate matter, these small animals also developed more advanced coronary lesions (with an increase in lipid deposition) and extensive atherosclerosis in the aorta, as compared to the rabbits that were not exposed [24]. The American Heart Association has also released an important guiding statement grounded on scientific data, warning about the short-term and long-term impacts of PM2.5 exposure on cardiovascular health, mortality, and life expectancy [25].
Ozone is present in two separate layers of the atmosphere. Stratospheric ozone (in the upper atmospheric layer) is protective and works as a shield for the biosphere against harmful ultraviolet rays from the sun. Tropospheric or ground-level ozone, on the other hand, poses a direct hazardous risk to the health of children, elderly individuals, and people with underlying respiratory, cardiovascular, and neurological conditions. Ground-level ozone is mostly produced due to the pollution emitted from automobiles, power plants, industrial boilers, refineries, and chemical plants, and is increasing in prevalence at a considerable rate. In addition to being a major air pollutant, ozone is also a potent greenhouse gas that contributes to climatechange, and thus can further impact human health.
The oxidative nature of ozone makes it capable of reacting with a large range of cellular components and body tissues, especially those in the respiratory airways and lungs. As a result of ozone inhalation, lipids and proteins on the surface of cells and in the lung-lining fluid interact with it, and the airway lining can become thinner, shrinking to 10 µm in major airways and 0.2 µm in the alveolar region. Ozone damages epithelial cells lining the respiratory tract, causing them to leak intracellular enzymes, such as lactate dehydrogenase, and plasma components into the airway lumen. Various studies have concluded that polymorphonuclear leukocytes (PMNs) can be attracted to the lung by these leaked chemicals and other inflammatory mediators released by the epithelial cells, which can also activate alveolar macrophages and initiate a series of events that can result in severe inflammation of the lung [26,27]. Exposure to ambient ozone is linked to triggering acute and chronic health effects [28,29]. Potentially harmful effects of ozone involve chest discomfort, coughing, shortness of breath, and rising daily ozone concentrations are associated with increased asthma attacks, hospitalizations, deaths, and other markers of morbidity [30]. Patients with pre-existing respiratory diseases are at elevated risk of suffering the effects of ozone exposure for two possible reasons, either their response to ozone may interact with the pathophysiology of the disease they are already suffering from or because they have a lower pulmonary function, they cannot tolerate a further reduction in it due to ozone exposure [27].
Ozone has been a long-term interest of researchers who have been trying to figure out its relationship with airway diseases. Studies conducted initially in rats and mice, and later in humans, revealed that bronchial hyperresponsiveness accompanied by a neutrophilic inflammation was a result of acute exposure to ozone. Also, chronic exposure to ozone has allowed researchers to create a good model of emphysema and chronic airway inflammation. This has gained tremendous attention in recent years. These studies have provided the strongest evidence that ozone induced oxidative stress could lead to features similar to those found in chronic obstructive pulmonary disease (COPD) [31]. Furthermore, researchers have shown that COPD patients while doing light exercises show slight decreases in arterial blood oxygen saturation after exposure to 300 ppb of ozone for two hours. Even though it is unclear if these changes in oxygen saturation caused by ozone exposure can lead to worsening COPD and the need for immediate hospitalization, people with chronic respiratory diseases and COPD should avoid strenuous outdoor activity during high ozone concentrations [27].
Ozone and particulate matter are currently considered to be the most detrimental pollutants with respect to effects on morbidity and mortality. 4,200,000 deaths and 103,000,000 life years of healthy living lost (due to disability) were linked to atmospheric particulate matter alone, with another 254,000 deaths and 4,100,000 disability-adjusted life years linked to ozone [32]. According to recent findings, one of the early biological responses triggered by the inhalation of these pollutants is a stress response, through the activation of the hypothalamic-pituitary-adrenal (HPA) axis and the resulting release of the stress hormones [33]. In many chronic health conditions, such as cognitive disorders, depression, and metabolic diseases, dysregulation of the HPA axis has been noted to be a characteristic feature. The brain responds to pollutants that trigger stress axis activation. In response to ozone and particulate matter, the pituitary gland releases adrenocorticotropic hormone, which in turn causes the adrenal glands to release glucocorticoids (GC), most notably cortisol. The GC hormone binds to its receptors (GR) to regulate processes, such as glucose and lipid metabolism, and immune and inflammatory functions, as well as response to other hormones. As stress hormones are released, the levels of inflammatory mediators in the blood (e.g., cytokines and other reactive metabolic products) change, which also impacts the brain, lungs, and peripheral tissues. This chronic activation and dysregulation of the HPA axis results in neurotoxicity, oxidative stress sensitization, and impaired control of inflammation. Together, these effects interact with individual susceptibility to contribute to malignant diseases manifesting within the body and the brain [33]. There is an increasing body of evidence linking these air pollutants with brain health and disorders, including impaired cognitive performance [34-36], dementia [37], anxiety and depression [38,39], and suicide [40,41].
The increase in global temperatures is directly affecting plant pollen production worldwide as the increasing carbon dioxide levels and warmer temperatures contribute to higher proliferation of many plants, including the allergenic ones such as ragweed, sagebrush, pigweed, lambs’ quarters, and tumbleweed, which affect more than 23 million people in the United States. For instance, higher pollen production and lengthened pollen seasons can be attributed to both higher spring temperatures and later first fall-frosting in central North America. An experimental study was conducted by growing ragweed concurrently in urban and rural environments. In the urban environment, where the carbon dioxide concentrations were 30% higher than in the rural environment, ragweed grew much faster, flowered earlier, and produced greater aboveground biomass and pollen compared to the rural environment [42]. Studies of pollen seasons in Europe have also shown earlier starts in London, Brussels, Zurich, and Vienna [43]. It has been approximated that by 2041-2060, 33 to 77 million Europeans will suffer from ragweed allergy. The most notable increases in ragweed sensitization will occur in countries with little or no current such issue, such as Germany, Poland, and France [44].
Other than ragweed pollen allergies, some studies have also linked climate change to mold allergies, especially after flooding and other extreme weather events when standing water and water intrusion encourages mold growth. In a study conducted by Lang-Yona et al. in 2013, Aspergillus fumigatus spores were cultured in different growth environments with increasing atmospheric CO2 concentrations to investigate the changes in its allergenicity as a function of atmospheric CO2 concentration [45]. Mold grown in conditions similar to the current global atmospheric carbon dioxide levels produced 8.5 times more allergenic protein as compared to those grown under pre-industrial carbon dioxide levels, due to higher rates of fungal growth and respiration. These results provide evidence that the sharp rise in atmospheric carbon dioxide emissions can also worsen allergic responses related to fungal growth.
In addition to increasing the concentration of pollen in the air, global warming also increases the potency of airborne allergens to induce allergies. According to a study on the impact of urbanization on the proteome of birch pollen and its effect on human granulocytes, extracts from birch pollen collected in urban areas were highly active in stimulating the chemotaxis of human neutrophils [46]. Another study found exposure to ozone as a key factor that contributes to the allergenic nature of birch pollen in susceptible individuals. Besides its direct impact on respiratory health, ozone can also cause allergic symptoms by increasing allergenicity [47]. Pollen can travel a long distance from its source due to climate change and the increasing wind intensities [44]. Accordingly, aeroallergens and global climate change have been closely linked in the recent reports of the American Academy of Allergy, Asthma & Immunology Working Group. As pollen seasons become longer, human exposure to allergens will increase, and so will allergic sensitization. Over the past few years, emergency visits and hospital admissions for asthma and allergic rhinitis, as well as physician visits and sales of over-the-counter allergy medications have increased [46].
According to the World Health Organization (WHO), an estimated 10 million people suffered from tuberculosis (TB) worldwide in 2020 (5.6 million men, 3.3 million women and 1.1 million children) [48]. Even though TB is mostly treatable and preventable, ~1.5 to 2 million individuals die from TB every year and new drug-resistant strains have been on the rise since the last two decades, posing a serious global health problem. Mycobacterium tuberculosis, the causative agent of TB, is an intracellular pathogen and typically resides in the lungs, producing breathing difficulties and characteristic tissue lesions in the alveoli called ‘granulomas’ [49]. TB is a highly contagious disease and can spread from person to person through the coughing, sneezing, and spitting of an infected patient with active pulmonary TB, which releases the pathogenic mycobacteria in the form of easily inhalable aerosols in the air. Mycobacteria are mesophilic and grow optimally at moderate to high temperatures (up to 45°C). Colder temperatures, on the other hand, reduce their metabolic functions and M. tuberculosis cannot multiply efficiently in low oxygen environments. This can explain why people living in high altitude areas are affected by a lower incidence and spread of TB than those at lower altitudes or near the coast. It has been observed that TB prevalence fluctuates in different geographical regions based on the altitude and temperature conditions, particularly for pulmonary TB [50]. Additionally, hot weather contributes to an environment conducive to TB spread due to the high rate of airflow. Air quality is also influenced by increasing levels of polluting gases, including carbon monoxide, which induces bacillary reactivation and increases the incidence of TB [51].
TB has been recognized as a significant infectious disease linked to climate change in the recent years [52-54]. A study conducted in China showed a seasonal pattern of new TB cases reaching their utmost in late spring to early summer and their lowest in late winter to early spring [55]. In a previous study conducted in Cameroon, significantly more TB cases were reported during the rainy seasons, relative to other seasons. TB outbreaks have also been associated with relatively low humidity. The results of a study carried out for three districts of Bangladesh between 2007 and 2012, present a strong association between the three climate variables of temperature, humidity, and rainfall, and the net TB incidence. A cyclic pattern was observed in the changes of the three weather factors during this time period, with moderate temperature, low humidity and moderate rainfall favoring higher number of TB cases in all the three districts [56].
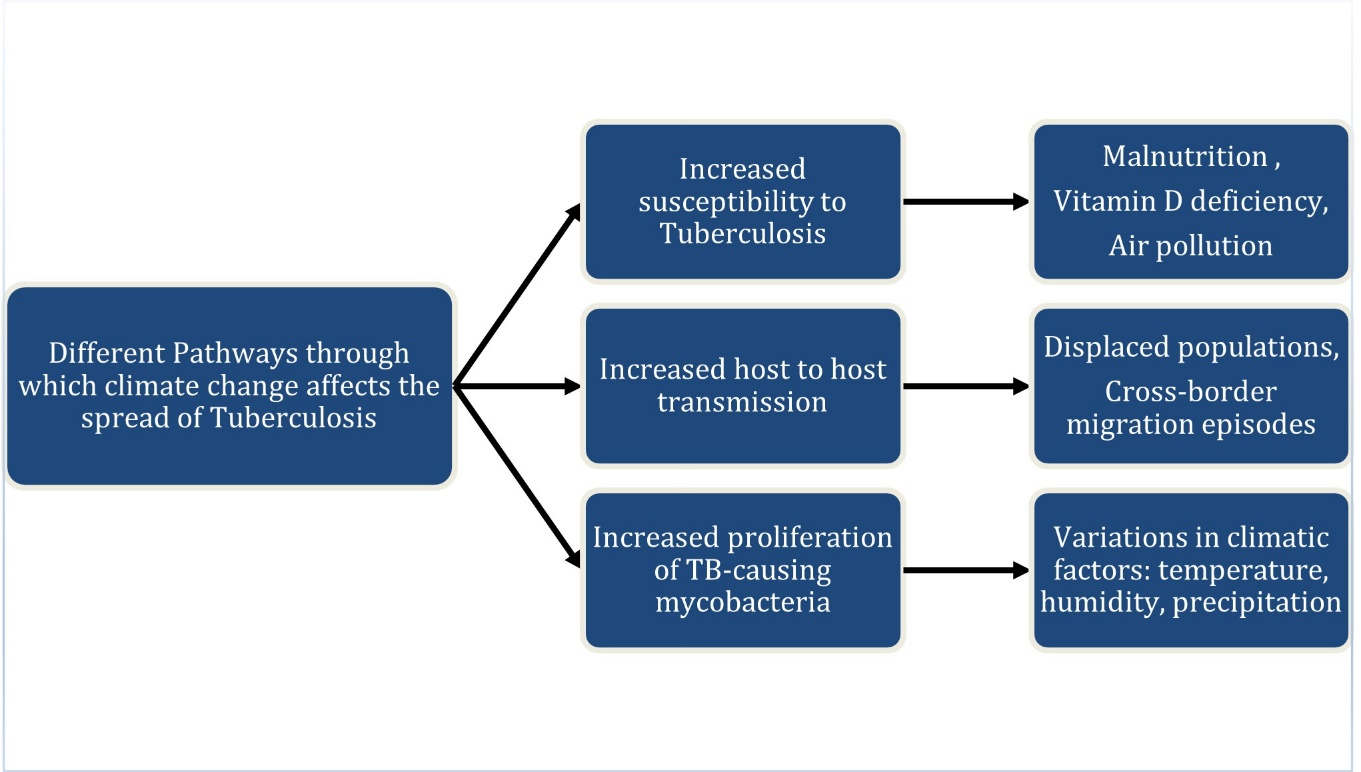
Figure 1: Schematic summarizing the three different pathways through which climate change is affecting the spread of Tuberculosis (TB) globally: 1) Increased susceptibility to Tuberculosis, 2) Increased host to host transmission, and 3) Increased proliferation of mycobacteria. To the right of each pathway, various causal factors that lead to it are indicated via a horizontal arrow.
Other complicated pathways also affect the spread of TB disease, which has been a global pandemic for the last 50 years. As summarized in Figure 1, we have investigated the various factors that connect global climate change with the increasing incidence of TB. Another critical way in which climate change affects the TB pandemic is through its impact on food security and nutrition. Climate change is causing substantial changes in yield and area growth, higher food prices and therefore, a reduction in affordability of food, reduced calorie availability, and more malnutrition in multiple countries, especially Sub-Saharan Africa [57]. Food security poses another big threat in areas like Bangladesh and Vietnam that are under rising sea levels, as saltwater is more likely to flood coastal farmlands. The United States Department of Agriculture (USDA) reports that Vietnam is the world's second largest exporter of rice, and 80% of the net production is grown in the Mekong Delta, a vast floodplain and one of Asia's most fertile agricultural areas, and thus a flood in this region could affect both the country's food security and economy [58]. Studies have also indicated that salinity issues in other countries, such as Bangladesh, will most likely lead to significant shortages of drinking water and irrigation by 2050. In this case, increased soil salinity may result in a drop in rice yield by about 15.6%, thereby significantly reducing the income of affected farmers. Among countries with high TB burden, including India, China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa, undernutrition remains the most significant cause of TB over the decades, and both undernutrition and malnutrition increase the risk of developing severe TB disease and mortality [48,59]. In particular, Vitamin D deficiency is associated with a higher risk of active TB [60]. Several factors threaten food production for smallholder farmers, such as irregular rains, extreme weather events, higher temperatures, and saltwater infiltration from rising sea levels, leading to decreased crop yields [61]. Additionally, impaired water quality resulting from extreme weather events like floods and cyclones can lead to infectious diarrhea and parasitic infections, increasing undernutrition among vulnerable people [62]. Malnutrition spikes are also triggered by climate shocks that restrict food access [63]. By predicting and mitigating the effects of climate on food availability, food access and water quality, TB diminution and elimination efforts could be made more effective in countries with high TB incidence.
Furthermore, according to International Organization for Migration (IOM), TB risk is particularly higher for migrants of specific social and legal status, such as workers, undocumented migrants, trafficked and detained persons. Migrants are more susceptible to TB infection due to overcrowded living and working conditions, malnutrition, and substance abuse due to marginalization and social exclusion [64].
Climate impacts weather, air and water quality, local and national food supply chains, economics, and many other critical health factors. Many parts of the world are experiencing regional changes in climate, especially temperature spikes and extreme weather events. This affects a large variety of physical and biological systems. Changes in infectious disease transmission patterns are an inevitable consequence of climate change. It is essential to identify the causal relationships and use this knowledge to predict future emerging risks using more complete, better validated, and integrated models. Different governments, non-governmental organizations, charitable foundations, and research teams need to collaborate effectively to address this health crisis facing us and come up with practical coping strategies. More funding and research need to be scaled up accordingly at a much faster rate.
Studies are increasingly showing the interrelated nature of social and economic impacts of climate change on the health of people. Developing countries and communities with low income are particularly vulnerable to climate change. The poor have a much higher possibility of experiencing the negative effects of climate change since they are more exposed and have fewer resources or limited ability to cope with them [65]. Compared to the economically stable and developed countries where climate change has largely been a matter of dealing with longer, hotter summers and the observed seasonal changes, poorer countries often experience crippling economic shocks as a result of weather-related disasters, poor harvests, or even the illness of the household members [66]. Due to extreme weather events like cyclones, storm surges, floods, and droughts, 26 million people currently fall into poverty each year, resulting in $520 billion loss in consumption globally. It is estimated that climate change is likely to pull up to 132 million people into extreme poverty by 2030 through its impacts on agricultural productivity and consequently lowered agricultural incomes, increased food prices for the consumers, reduced labor productivity and their incomes, and increases in zoonoses and water- or vector-borne diseases [67]. Accordingly, climate change is also negatively affecting social factors, such as equality and access to health care and social support structures, which can pose further health risks especially for the most vulnerable, including women, children, poor and malnourished communities, aging populations, and migrants or displaced populations.
| Climate Change-related Health Risks | Specific diseases | Affected geographical regions | References |
|---|---|---|---|
| Vector-borne Diseases |
Dengue Malaria Yellow Fever Chikungunya Zika |
Tropical and Subtropical Regions (Kenya, Malawi, Tanzania, Amazon Region, Mekong Delta Subregion, the Caribbean, the Pacific islands) | [3], [4], [5] |
| Water-borne diseases | Cholera | East Africa, Zambia, South China, Iran | [14], [16], [17], [18] |
| Cardiovascular diseases |
Congestive Heart Failure (CHF) Acute Myocardial Infarction (AMI) |
Canada, United States, Europe | [19], [23] |
| Respiratory Diseases |
Asthma Attacks Chronic Obstructive Pulmonary Disease (COPD) |
United Kingdom, France, Germany, Italy South-East Asia, Central Africa and Western Pacific region, China | [30], [31], [42], [48], [54], [55], [58] |
|
Allergies Tuberculosis |
United States, Europe Cameroon, Bangladesh, India, China, Indonesia, The Philippines, Pakistan, Nigeria, South Africa |
||
| Neurological diseases |
Cognitive Disorders Depression Metabolic Diseases Dysregulation of The HPA Axis Dementia Anxiety Suicide |
United States, Canada, South Korea, Taiwan | [33], [37], [38], [39], [40], [41] |
Among the top ten leading causes of death which accounted for 55% of the 55.4 million deaths globally in 2019 [68], seven categories include the various communicable and non-communicable diseases we have discussed in the aforementioned sections, which are directly influenced by climate change, such as cardiovascular (ischemic heart disease, stroke), respiratory (COPD, TB, lower respiratory infections), diarrheal diseases, dementia, and other neurological disorders. Furthermore, with global warming the burden of vector-borne diseases is continuously increasing worldwide, acting as another major cause of death and illness. For instance, from 2004 to 2016, disease cases from mosquitoes, ticks, and fleas in the United States nearly tripled from just under 30,000 to almost 100,000 [69]. In general, the tropical and subtropical parts of the world are more severely struck by various vector-borne diseases, such as Dengue, Malaria, Zika and Chikungunya. We have listed various geographical regions which have been adversely affected by the different diseases in Table 1, and a global picture of serious health risks is apparent. In the recent years, WHO has also focused on providing guidance on how to conduct national or subnational assessment of current and future vulnerability of the different populations to various kinds of climate-related health effects and the associated adaptation analyses [70]. It is imperative to identify weaknesses in the systems that need specific interventions, while carefully considering the multiple determinants of climate-sensitive health outcomes. Future adaptation measures should entail implementation of policies and programs that could increase resilience of the populations to various climate-related health risks.
This research was supported by the NIH Bridges grant 1T34GM137858 (NIGMS). Dr. Richa Gupta served as the Principal Investigator and Research Mentor, and Sara El Houzaly was supported by the NIH Bridges Undergraduate Research Scholarship through it.
[1] IPCC, 2021: Summary for Policymakers. In: Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [V. MassonDelmotte, P. Zhai, A. Pirani, S.L. Connors, C. Péan, S. Berger, N. Caud, Y. Chen, L. Goldfarb, M.I. Gomis, M. Huang, K. Leitzell, E. Lonnoy, J.B.R. Matthews, T.K. Maycock, T. Waterfield, O. Yelekçi, R. Yu, B. Zhou. Cambridge University Press 2021.
[2] NASA Global Climate Change: Evidence (2022). https://climate.nasa.gov/evidence/
[3] IPCC Climate Change 2013: The Physical Science Basis. In: Stocker TF, Qin D, Plattner G-Ket al. (eds). Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change, Cambridge, UK:Cambridge University Press 2013, 1535.
[4] Ogden NH. Climate change and vector-borne diseases of public health significance. FEMS Microbiol Lett 2017; 364(19).
[5] Ngarakana-Gwasira ET, Bhunu CP, Masocha M, Mashonjowa E. Assessing the Role of Climate Change in Malaria Transmission in Africa. Malar Res Treat 2016; 7104291.
[6] WHO (World Health Organization), 2020. Fact sheet about malaria. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/malaria
[7] Bouma MJ, Dye C. Cycles of malaria associated with El Niño in Venezuela 1997; 278(21):1772-4.
[8] Small J, Goetz SJ, Hay SI. Climatic suitability for malaria transmission in Africa, 1911-1995. Proc Natl Acad Sci U S A 2003; 100(26):15341-5.
[9] Haider M, Turner J. Variables that may affect the transmission of dengue – A case study for Health Management in Asia. Topics in Public Health, Dr. David Claborn 2015.
[10] Tran BL, Tseng WC, Chen CC, Liao SY. Estimating the Threshold Effects of Climate on Dengue: A Case Study of Taiwan. Int J Environ Res Public Health 2020; 17(4):1392.
[11] Levy K, Smith SM, Carlton EJ. Climate Change Impacts on Waterborne Diseases: Moving Toward Designing Interventions. Curr Environ Health Rep 2018; 5(2):272-282.
[12] Ali M, Nelson AR, Lopez AL, Sack DA. Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis 2015; 9(6):e0003832.
[13] Pandey PK, Kass PH, Soupir ML, Biswas S, Singh VP. Contamination of water resources by pathogenic bacteria. AMB Express 2014; 4:51.
[14] Escobar LE, Ryan SJ, Stewart-Ibarra AM, Finkelstein JL, King CA, Qiao H et al. A global map of suitability for coastal Vibrio cholerae under current and future climate conditions. Acta Trop 2015; 149:202-11.
[15] Asadgol Z, Mohammadi H, Kermani M, Badirzadeh A, Gholami M. The effect of climate change on cholera disease: The road ahead using artificial neural network. PLoS One 2019;14(11):e0224813.
[16] Olago D, Marshall M, Wandiga SO, Opondo M, Yanda PZ, Kanalawe R et al. Climatic, socio-economic, and health factors affecting human vulnerability to cholera in the Lake Victoria basin, East Africa. Ambio 2007; 36(4):350-8.
[17] Luque Fernández MA, Bauernfeind A, Jiménez JD, Gil CL, El Omeiri N, Guibert DH. Influence of temperature and rainfall on the evolution of cholera epidemics in Lusaka, Zambia, 2003-2006: analysis of a time series. Trans R Soc Trop Med Hyg 2009; 103(2):137-43.
[18] Yue Y, Gong J, Wang D, Kan B, Li B, Ke C. Influence of climate factors on Vibrio cholerae dynamics in the Pearl River estuary, South China. World J Microbiol Biotechnol 2014; 30(6):1797-808.
[19] Bai L, Shin S, Burnett RT, Kwong JC, Hystad P, van Donkelaar A et al. Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: A population-based study of 5.1 million Canadian adults living in Ontario. Environ Int 2019; 132:105004.
[20] Franchini M, Mannucci PM. Thrombogenicity and cardiovascular effects of ambient air pollution. Blood 2011; 118(9):2405-12.
[21] Cahill TJ, Kharbanda RK. Heart failure after myocardial infarction in the era of primary percutaneous coronary intervention: Mechanisms, incidence and identification of patients at risk. World J Cardiol 2017; 9(5):407-415.
[22] Du Y, Xu X, Chu M, Guo Y, Wang J. Air particulate matter and cardiovascular disease: the epidemiological, biomedical and clinical evidence. J Thorac Dis. 2016; 8(1):E8-E19.
[23] Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M et al. Expert Panel on Population and Prevention Science of the American Heart Association. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 2004; 109(21):2655-71.
[24] Franklin BA, Brook R, Arden Pope C 3rd. Air pollution and cardiovascular disease. Curr Probl Cardiol 2015; 40(5):207-38.
[25] Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV et al. American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010; 121(21):2331-78.
[26] Cheng W, Duncan KE, Ghio AJ, Ward-Caviness C, Karoly ED, Diaz-Sanchez D et al. Changes in Metabolites Present in Lung-Lining Fluid Following Exposure of Humans to Ozone. Toxicol Sci 2018; 163(2):430-439.
[27] US EPA (United States Environmental Protection Agency website), 2021. Health Effects of Ozone in the General Population. https://www.epa.gov/ozone-pollution-and-your-patients-health/health-effects-ozone-general-population
[28] Wang M, Sampson PD, Sheppard LE, Stein JH, Vedal S, Kaufman JD. Long-Term Exposure to Ambient Ozone and Progression of Subclinical Arterial Disease: The Multi-Ethnic Study of Atherosclerosis and Air Pollution. Environ Health Perspect 2019; 127(5):57001.
[29] Zhang JJ, Wei Y, Fang Z. Ozone Pollution: A Major Health Hazard Worldwide. Front Immunol 2019; 10:2518.
[30] Tiotiu AI, Novakova P, Nedeva D, Chong-Neto HJ, Novakova S, Steiropoulos P et al. Impact of Air Pollution on Asthma Outcomes. Int J Environ Res Public Health 2020; 17(17):6212.
[31] Wiegman CH, Li F, Ryffel B, Togbe D, Chung KF. Oxidative Stress in Ozone-Induced Chronic Lung Inflammation and Emphysema: A Facet of Chronic Obstructive Pulmonary Disease. Front Immunol 2020; 11:1957.
[32] Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017 May 13;389(10082):1907-1918.
[33] Thomson EM. Air Pollution, Stress, and Allostatic Load: Linking Systemic and Central Nervous System Impacts. J Alzheimers Dis 2019; 69(3):597-614.
[34] Zhang X, Chen X, Zhang X. The impact of exposure to air pollution on cognitive performance. Proc Natl Acad Sci U S A 2018; 115(37):9193-9197.
[35] Chen JC, Schwartz J. Neurobehavioral effects of ambient air pollution on cognitive performance in US adults. Neurotoxicology 2009; 30(2):231-9.
[36] Gatto NM, Henderson VW, Hodis HN, St John JA, Lurmann F, Chen JC et al. Components of air pollution and cognitive function in middle-aged and older adults in Los Angeles. Neurotoxicology 2014; 40:1-7.
[37] Chen H, Kwong JC, Copes R, Hystad P, van Donkelaar A, Tu K et al. Exposure to ambient air pollution and the incidence of dementia: A population-based cohort study. Environ Int 2017; 108:271-277.
[38] Kioumourtzoglou MA, Power MC, Hart JE, Okereke OI, Coull BA, Laden F et al. The Association Between Air Pollution and Onset of Depression Among Middle-Aged and Older Women. Am J Epidemiol 2017; 185(9):801-809.
[39] Pun VC, Manjourides J, Suh H. Association of Ambient Air Pollution with Depressive and Anxiety Symptoms in Older Adults: Results from the NSHAP Study. Environ Health Perspect 2017; 125(3):342-348.
[40] Kim Y, Ng CFS, Chung Y, Kim H, Honda Y, Guo YL et al. Air Pollution and Suicide in 10 Cities in Northeast Asia: A Time-Stratified Case-Crossover Analysis. Environ Health Perspect 2018; 126(3):037002.
[41] Szyszkowicz M, Willey JB, Grafstein E, Rowe BH, Colman I. Air pollution and emergency department visits for suicide attempts in vancouver, Canada. Environ Health Insights 2010; 4:79-86.
[42] Ziska L, Knowlton K, Rogers C, Dalan D, Tierney N, Elder MA et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc Natl Acad Sci U S A 2011; 108(10):4248-51.
[43] Emberlin J, Detandt M, Gehrig R, Jaeger S, Nolard N, Rantio-Lehtimäki A. Responses in the start of Betula (birch) pollen seasons to recent changes in spring temperatures across Europe. Int J Biometeorol 2002; 46(4):159-70.
[44] Lake IR, Jones NR, Agnew M, Goodess CM, Giorgi F, Hamaoui-Laguel L, Semenov MA, Solmon F, Storkey J, Vautard R, Epstein MM. Climate Change and Future Pollen Allergy in Europe. Environ Health Perspect 2017; 125(3):385-391.
[45] Lang-Yona N, Levin Y, Dannemiller KC, Yarden O, Peccia J, Rudich Y. Changes in atmospheric CO2 influence the allergenicity of Aspergillus fumigatus. Glob Chang Biol 2013; 19(8):2381-8.
[46] Joshi M, Goraya H, Joshi A, Bartter T. Climate change and respiratory diseases: a 2020 perspective. Curr Opin Pulm Med 2020; 26(2):119-12.
[47] Beck I, Jochner S, Gilles S, McIntyre M, Buters JT, Schmidt-Weber C et al. High environmental ozone levels lead to enhanced allergenicity of birch pollen. PLoS One 2013;8(11): e80147.
[48] WHO (World Health Organization), 2021. Tuberculosis (TB). https://www.who.int/news-room/fact-sheets/detail/tuberculosis
[49] Sheedy FJ, Divangahi M. Targeting immunometabolism in host defense against Mycobacterium tuberculosis. Immunology 2021;162(2):145-159.
[50] Gelaw YA, Yu W, Magalhães RJS, Assefa Y, Williams G. Effect of Temperature and Altitude Difference on Tuberculosis Notification: A Systematic Review. J Glob Infect Dis 2019; 11(2):63-68.
[51] Fernandes FMC, Martins ES, Pedrosa DMAS, Evangelista MDSN. Relationship between climatic factors and air quality with tuberculosis in the Federal District, Brazil, 2003-2012. Braz J Infect Dis 2017; 21(4):369-375.
[52] Wingfield T, Schumacher SG, Sandhu G, Tovar MA, Zevallos K, Baldwin MR et al. The seasonality of tuberculosis, sunlight, vitamin D, and household crowding. J Infect Dis 2014; 210(5):774-83.
[53] Leung CC, Yew WW, Chan TY, Tam CM, Chan CY, Chan CK et al. Seasonal pattern of tuberculosis in Hong Kong. Int J Epidemiol 2005; 34(4):924-30.
[54] Willis MD, Winston CA, Heilig CM, Cain KP, Walter ND, Mac Kenzie WR. Seasonality of tuberculosis in the United States, 1993-2008. Clin Infect Dis. 2012; 54(11):1553-60.
[55] Liu L, Zhao XQ, Zhou Y. A tuberculosis model with seasonality. Bull Math Biol 2010; 72(4):931-52.
[56] Kuddus MA, McBryde ES, Adegboye OA. Delay effect and burden of weather-related tuberculosis cases in Rajshahi province, Bangladesh, 2007-2012. Sci Rep 2019; 9(1):12720.
[57] Ringler C, Zhu T, Cai X, Koo J, Wang D. Climate change impacts on food security in Sub-Saharan Africa: Insights from comprehensive climate change scenarios 2010.
[58] Renaud FG, Thi Thu Huong L, Lindener C, Thi Guong V, Sebesvari Z. "Resilience and shifts in agro-ecosystems facing increasing sea-level rise and salinity intrusion in Ben Tre Province, Mekong Delta" Climatic change 2015; 69-84.
[59] Sinha P, Lönnroth K, Bhargava A, Heysell SK, Sarkar S, Salgame P et al. Food for thought: addressing undernutrition to end tuberculosis. Lancet Infect Dis 2021; 21(10):e318-e325.
[60] Aibana O, Huang CC, Aboud S, Arnedo-Pena A, Becerra MC, Bellido-Blasco JB et al. Vitamin D status and risk of incident tuberculosis disease: A nested case-control study, systematic review, and individual-participant data meta-analysis. PLoS Med 2019; 16(9):e1002907.
[61] Bandara JS, Cai Y. "The impact of climate change on food crop productivity, food prices and food security in South Asia," Economic Analysis and Policy, Elsevier 2014.p.451-465.
[62] Maharjan B, Gopali RS, Zhang Y. A scoping review on climate change and tuberculosis. Int J Biometeorol 2021; 65(10):1579-1595.
[63] Niles MT, Salerno JD. A cross-country analysis of climate shocks and smallholder food insecurity. PLoS One 2018; 13(2):e0192928.
[64] IOM (International Organization for Migration), 2012. Migration & Tuberculosis: A pressing issue. https://www.iom.int/sites/g/files/tmzbdl486/files/migrated_files/What-We-Do/docs/Migration-Tuberculosis-A-Pressing-Issue.pdf
[65] Rayner S, Malone EL. Climate change, poverty, and intragenerational equity: the national level. International Journal of Global Environmental Issues 2001; 1 (2): 175–202.
[66] UNDP (United Nations Development Programme), 2006. Human Development Report 2006: Beyond scarcity: Power, poverty and the global water crisis. New York. Palgrave Macmillan. https://hdr.undp.org/content/human-development-report-2006
[67] Jafino BA, Walsh B, Rosenberg J, Hallegatte S. Revised Estimates of the Impact of Climate Change on Extreme Poverty by 2030. Policy Research Working Paper 2020; 9417. World Bank, Washington, DC. ©World Bank. https://openknowledge.worldbank.org/handle/10986/34555
[68] WHO (World Health Organization), 2020. The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
[69] Rosenberg R, Nicole P, Fischer M, Gregory C, Hinckley A, Mead P et al. Vital signs: trends in reported vectorborne disease cases–United States and territories, 2004–2016. MMWR Morb Mortal Wkly Rep 2018; 67:496–501.
[70] WHO (World Health Organization), 2013. Protecting health from climate change: vulnerability and adaptation assessment. World Health Organization. https://apps.who.int/iris/handle/10665/104200